Our depth of experience in brachial plexus injuries
The Brachial Plexus Program at Boston Children’s Hospital provides comprehensive care for babies, children, adolescents, and young adults with brachial plexus injuries. We follow our patients from the time of injury to young adulthood, tailoring treatments to assure each of our patients achieve the highest level of function and independence possible.
We treat children with all types of brachial plexus injuries, including:
- Brachial plexus birth injury (BPBI)
- Traumatic brachial plexus injury
- Erb’s palsy
- Total plexus involvement
- Horner’s syndrome
- Klumpke’s palsy
- Acute flaccid myelitis
- Thoracic outlet syndrome
Expertise in brachial plexus repair
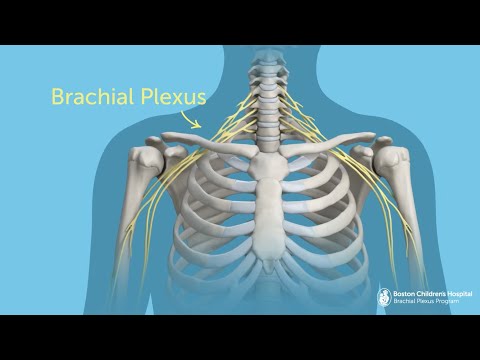
The brachial plexus is a network of nerves that run from the spinal cord in the neck to the shoulder, arm, and hand. These nerves can be damaged during a difficult birth or as the result of trauma that forcibly pulls or stretches this part of the upper body. In either case, brachial plexus injury can cause weakness, numbness, or full or partial paralysis in the affected arm.
Treatment of brachial plexus injuries requires a unique combination of expertise in orthopedic surgery and nerve repair. Our team has deep experience reconstructing damaged nerves and restoring function to the muscles and joints that rely on those nerves for strength, sensation, and function.
Why choose the Brachial Plexus Program?
Our multidisciplinary team of surgeons, nurses, and therapists have cared for thousands of patients with brachial plexus injury. Our program stands virtually alone in providing the entire spectrum of brachial plexus care — from early nerve surgery, to early therapy, to later reconstructive orthopedic surgery and therapy if needed.
Nonsurgical and surgical treatments for brachial plexus injury
We often follow children with brachial plexus injury from birth through adulthood. With a child-centered approach, we provide our patients state-of-the-art treatment appropriate to their age, stage of development, and degree of injury. Our expertise includes:
- Observation
- Physical therapy and occupational therapy
- Microsurgery
- Osteotomy
- Tendon transfer
- Open and arthroscopic reduction of the shoulder joint
- Intraoperative neurophysiological monitoring
- Free muscle transfer
Brachial plexus research and innovation
Boston Children’s Brachial Plexus Program is a center for research and innovation in brachial plexus care and recovery. Our physicians have pioneered diagnostic and treatment methods used widely at children’s hospitals around the country today. For instance, the Waters classification system, developed at Boston Children’s by Dr. Peter Waters, helps orthopedic specialists determine the degree of shoulder joint involvement in brachial plexus injuries and make informed treatment decisions.
When to perform microsurgery on infants with brachial plexus injury
While it’s generally accepted that microsurgery benefits infants with significant brachial plexus injury or loss of function, there has been significant controversy regarding the ideal timing for microsurgery for children whose long-term outcomes are unknown. The Brachial Plexus Program’s long-term Treatment and Outcomes of Brachial Plexus Injury (TOBI) study of brachial plexus birth injury treatment found that babies had similar muscle recovery even when surgery was performed later than 6 months of age, setting the standard for timing of microsurgery across the country.
An alternative approach to nerve transfer
Nerve transfer is a popular treatment for severe brachial plexus injury. Most nerve transfer surgeries are performed through an opening at the back of the shoulder. This approach works well in many instances, but has limitations if surgeons need access to additional nerves. Surgeons at Boston Children’s describe an alternative approach, repairing nerves through an opening at the front of the shoulder. This technique, which they perform routinely, expands options for surgical brachial plexus repair.
Brachial plexus injury studies
Non-sedated MRI
The NAPTIME study (non-anesthetized plexus technique for infant MRI evaluation) is an ongoing multi-center study that aims to provide more accurate early information about whether an infant with brachial plexus birth injury will require nerve surgery. Investigators at Boston Children’s and several other brachial plexus centers have developed an MRI technique that does not require sedation or injection of a contrast agent.
The GUPI Study (Growing Up with a Plexus Injury)
While the physical limitations of growing up with BPBI are well-studied, researchers do not know whether or how these limitations affect patients’ quality of life. The GUPI study is an international multi-center study led by Boston Children’s, which aims to define patient-reported function and quality of life in children with BPBI. We hope to identify which aspects of growing up with this chronic condition are most problematic for our patients so we can address these areas through research, clinical care, and advocacy.


