Heart Transplant | Listing & Waiting
At the conclusion of an evaluation for heart transplant, the transplant-team cardiologist and heart-transplant coordinator will communicate results to you and your child. They will also communicate these findings to a child’s primary physician and cardiologist.
Generally, there are three possible outcomes from the evaluation:
- Heart transplant is contraindicated or not possible.
- There are other treatments or medications available that should be considered prior to heart transplant.
- Heart transplant is a treatment option.
In all of these situations, the heart transplant team will work with a child’s physicians and family to develop a coordinated care plan.
Listing for a heart transplant
Once you and the transplant team decide heart transplant is the most appropriate treatment option, the child will be “listed” on the national computer system, United Network of Organ Sharing (UNOS), as a potential transplant recipient. UNOS matches organ donors by weight and blood type and current medical need with individuals waiting for a new heart. The wait can be from days to months.
The goal during listing and waiting is to preserve a child’s current cardiac function and to ensure the best quality of life possible. The waiting period may include frequent visits to the hospital for periodic checkups and hospitalizations for changes in medications. It is also possible that a child will need to wait in the hospital where intravenous (by vein) medications are administered to support the heart’s functioning.
If medically needed, a ventricular assist device (VAD) is used to provide a bridge to heart transplant. Depending upon the type of VAD, the child may be at home or in hospital.
The heart transplant team will support the family during the waiting period. Our social worker and child psychologist are available for the family as needed.
Heart Transplant | Surgery & Hospital Stay
Heart transplant surgery
A donor heart can become available at any time of the day or night. Timing is critical. The child will need to be ready to go to the operating room within one to two hours upon arrival at the hospital.
The child will be admitted to the cardiac floor or cardiac intensive care unit (CICU) and be prepared for surgery. An electrocardiogram (EKG), chest X-ray, and blood tests will be done. The child will be seen by the surgeons, anesthesiologists, and cardiologists to discuss the upcoming procedure.
While the child is being prepared for the operating room, a surgical team is leaving to obtain the donor heart. The time of operation is planned to match the team’s arrival back at Boston Children’s Hospital.
The heart can’t live long outside the body, so it is important to remove the heart, transport it to our hospital, and then transplant the heart within a few hours.
The transplant operation involves removing the damaged heart from the child’s body and attaching the new heart. The transplant operation takes about four to six hours. For children with complex congenital heart disease, the operation can be more involved because of the abnormal anatomy and the scar tissue from previous operations.
Parents can wait in the CICU waiting room at night or in the main surgical waiting area during the day. We provide progress reports every few hours during the operation.
Care after surgery is very similar to other open-heart surgeries. The child will return from the operating room on a breathing machine (ventilator) with a breathing tube in the nose or mouth. The child will be on a cardiac monitor, have several IVs and other tubes and equipment, and will be in a private room in the CICU to protect from infection.
The average hospital stay is two to four weeks. Half the time is spent in the CICU and the other half on the cardiac floor. Patients go to a private room on the cardiac floor when they leave the CICU, where they continue recovery, are monitored for rejection and other problems, and have medications adjusted.
Possible complications after heart transplant
Rejection
Rejection is a normal reaction of the body to a foreign object. When a new heart is placed in a child’s body, the body sees the transplanted organ as a threat and tries to attack it.
The immune system is responsible for the body’s defense against infection (such as bacteria or viruses) or foreign tissues (such as transplanted organs). A heart transplant is viewed by the body’s immune system as foreign, which means the body mounts an attack against the transplanted heart by sending cells from the immune system to destroy it. This attack is called rejection.
We can identify that rejection is occurring by looking at the cells in small pieces of the heart muscle (biopsy) under a microscope. We see swelling or inflammation around the heart’s muscle cells.
Following transplantation, immunosuppressive medications are used to prevent the immune system from rejecting the new heart. These medications are taken multiple times per day. Medicine to prevent rejection will be needed for the rest of a child’s life. Rejection of a transplanted organ will occur at unpredictable times following transplant. It is not a complication of the operation.
The chance of rejection is highest in the first few months after the heart transplant. The first year following transplant is the time period when we are working to establish the best combination of anti-rejection medications. A child may experience rejection but have no observable symptoms. However, there is often some evidence of rejection if a child experiences at least some the following symptoms:
- Fatigue
- Irritability
- Shortness of breath
- Difficulty breathing
- Fast heartbeat
- Irregular heartbeat
- Poor eating
- Decreased appetite
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Fever
We often treat rejection episodes in the first few months after transplant with hospitalization and high IV doses of immunosuppressive medication. Rejection episodes later in the transplant course may be treated with an increase in a child’s Prograf or CellCept or a course of oral prednisone for several days.
If the rejection is recurrent or more severe, additional immunosuppression may be necessary. We monitor children closely during rejection episodes. Cardiac biopsy will always be repeated following a rejection episode to see if the treatment was successful or if more treatment is needed.
Our goal is to give children adequate immunosuppression to prevent rejection but use the lowest doses possible to prevent side effects. Using drugs in combination allows us to use lower doses for each drug than if only one drug was used, so we generally take this approach to suppress a child’s immune response. Since every patient is different, finding a good balance takes some time, and many medication adjustments may be needed in the first few months.
Infection
Since children who undergo a heart transplant require medications that decrease their body’s immune system, they are at higher risk for infection. To some degree, a child will always be at higher risk of infection. However, a child will be at the highest risk early after transplant while on the highest doses of immunosuppressive medications.
The signs of an infection are similar to rejection. A child may develop:
- Fever
- Cough
- Irritability
- Diarrhea
- Vomiting
In addition, the wound from surgery may be red, swollen and draining.
Treatment is based on severity of symptoms and the cause of infection. Early post-transplant patients are often admitted to the hospital for both the evaluation of infection and treatment.
Going home after a heart transplant
Families will be taught their child’s current medication schedule, proper administration of the medication, and how to monitor for side effects and complications from the transplant.
In the beginning, the child will require frequent follow-up (once to twice per week). Families who live more than two hours from Boston are usually requested to stay in the local area for a period of time (six to 12 weeks) after discharge. Accommodations and length of stay after discharge will be determined on an individual basis.
Our goal after transplant is to return the child and their family to as normal a routine as possible. This will take time but will always remain our goal.
Heart Transplant | Long-Term Outlook
What is the long-term outlook following a heart transplant?
Living with a heart transplant is a journey, and each child and every transplant is different. Following the operation, the transplant team will see the child for frequent follow-up visits, initially once or twice per week in the Cardiology Clinic. Generally, after the first few months, this schedule will diminish. Usually, around one year following transplant, the frequency changes to every three to six months.
Most children will return to school approximately 10 to 12 weeks after surgery. However, many require special services, such as tutoring, in particular children who had complex congenital heart disease — a risk factor for learning problems.
The Boston Children's Hospital Cardiac Neurodevelopmental Program supports and works with children with heart disease. As a child settles into school, we closely monitor learning struggles. We can assist in obtaining educational assessments and interventions that can enhance a child’s academic achievement.
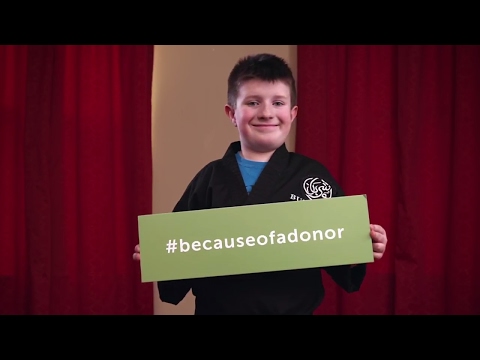
Aaron, 10, received a heart transplant at just 1 year old. #becauseofadonor, he was able to get his black belt.
Physical activity
We want and expect heart transplant recipients to live a fulfilling and productive life similar to other children their age. Before heart transplant, a child may not have been active; however, the activity level post-transplant will gradually increase.
Physical therapy will begin at the hospital, and an exercise program will be created that will integrate a child’s needs, goals, activity preferences, and home situation.
Warming up is very important after a heart transplant, as the heart now needs a few extra minutes to increase its rate. At the time of a child’s heart transplant, the main nerves to the heart are cut. This is known as denervation. Therefore, the brain does not directly control the heart rate. The body’s hormones that normally circulate in the blood system have less control over heart rate in a transplanted heart.
Medication adherence
Anti-rejection medications help the immune system accept the new heart. These medications must be taken for the lifetime of the transplanted organ.
Medication compliance is a major concern, particularly for teenagers as they seek more control of their lives and because of the temporary side effects caused by the drugs. Non-adherence may lead to rejection and loss of the heart, so it’s critical that medications are always taken as instructed, without missing doses.
The transplant coordinators and nurses work with teenagers and families to develop a medication schedule that fits the normal routine at home and creates a pattern that is easy to follow.
Nutrition
A nutritionist will help design a diet plan that promotes sound nutritional health and minimizes possible nutritional side effects of immunosuppressant therapy. Immunosuppressant medications can cause weight gain, salt retention, potassium loss, high blood sugar, and high blood pressure.
Designing a diet plan begins with obtaining, creating, and reviewing a nutrition history and determining a child’s ideal body weight. Using this information, a well-balanced diet is recommended that includes an appropriate number of calories, low sodium, and fats.
Growth and development following heart transplant
A child’s physical growth will be checked frequently, and we will make suggestions about diet changes or increasing calories as needed. We want your child to grow along his or her own growth curve following transplant.
We will also be carefully observing your child’s development at regular intervals and may make suggestions for additional services, such as early intervention and physical therapy, to enhance development. Although transplantation makes many extra demands on children, most children seem to adapt fairly well with help and support.



