At the Heart Failure and Transplant Program at Boston Children’s Hospital, our treatments are informed both by the current state of medical knowledge and by our own research. At Boston Children’s we are always looking for ways to improve and advance care.
Ventricular Assist Devices in children
In 2007, Boston Children’s Hospital cardiac surgeon Francis Fynn-Thompson, MD, received special permission from the United States Food and Drug Administration (FDA) to implant a Berlin Heart — a mechanical device that temporarily takes over the heart’s pumping functions — in a 9-year-old boy on the waiting list for a donor heart. This groundbreaking procedure saved the patient’s life.

That same year, the FDA allowed the nation’s first pediatric multi-center clinical trial of the Berlin Heart. Our cardiologists played a central role in designing the protocol. Four years and nearly 50 trial patients later — 90 percent of whom successfully transitioned to a transplanted heart after using the device — the FDA formally approved the use of the Berlin Heart in children of all ages experiencing end-stage heart failure.
Our cardiologists and cardiac surgeons have continued to identify mechanical and ventricular assist devices (VADs) of the future and to understand the optimum timing of device placement in children. The newer generation devices allow children to be discharged home, go to school and even play and have fun while they are waiting for a donor heart.
Reducing the number of biopsies for rejection monitoring
Our team is investigating if information obtained from a blood test and an ultrasound of the heart (echocardiogram) can be used to declare with high certainty that patient currently does not have rejection. If true, fewer routine biopsies would be needed to monitor patients after transplant — an idea our patients strongly support.
Thought leadership in heart organ allocation
Our cardiologists have written several original research papers that have studied the heart organ allocation system in the US. These papers influenced the direction of changes in national heart allocation such that sicker kids would be getting donor hearts more quickly.
Working with our peers across the country
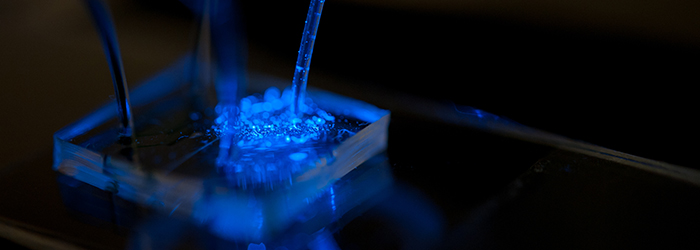
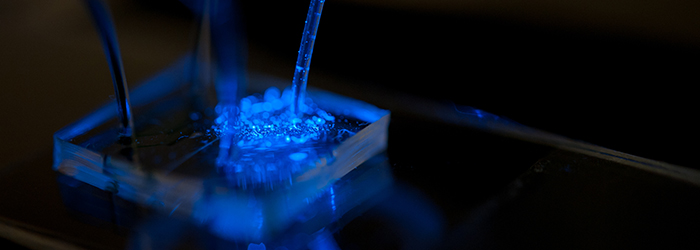
Boston Children’s Hospital is one of seven U.S. sites awarded a grant to study the outcomes of heart transplant in children who are highly sensitized (have antibodies against potential donors circulating in their blood). Children with congenital heart disease become ‘sensitized’ from the homograft material used to repair their heart. Historically, these patients had longer wait times and more risk of dying without receiving a heart. Our clinical protocol has allowed us to accept hearts even when patients have pre-existing antibodies against the donor. This is made possible by removing antibodies using plasmapheresis and neutralizing the effect of remaining antibodies using IVIG. Our NIH study is exploring the mechanisms behind this protocol.
In addition, the Heart Transplant Program clinicians participate in many other multi-center studies and registries, including the Pediatric Heart Transplant Study (PHTS), the Pediatric Cardiomyopathy Registry, ESLO (ECMO Registry), and INTERMACS and PEDIMACS Registries (for ventricular support devices). Our physicians and nurses have held leadership roles in PHTS, as co-principal investigator (co-PI) for PEDIMACS, as program chair for the International Society for Heart and Lung Transplantation and as site PI for many multi-center trials investigating heart failure, cardiomyopathy, VADs and transplantation.